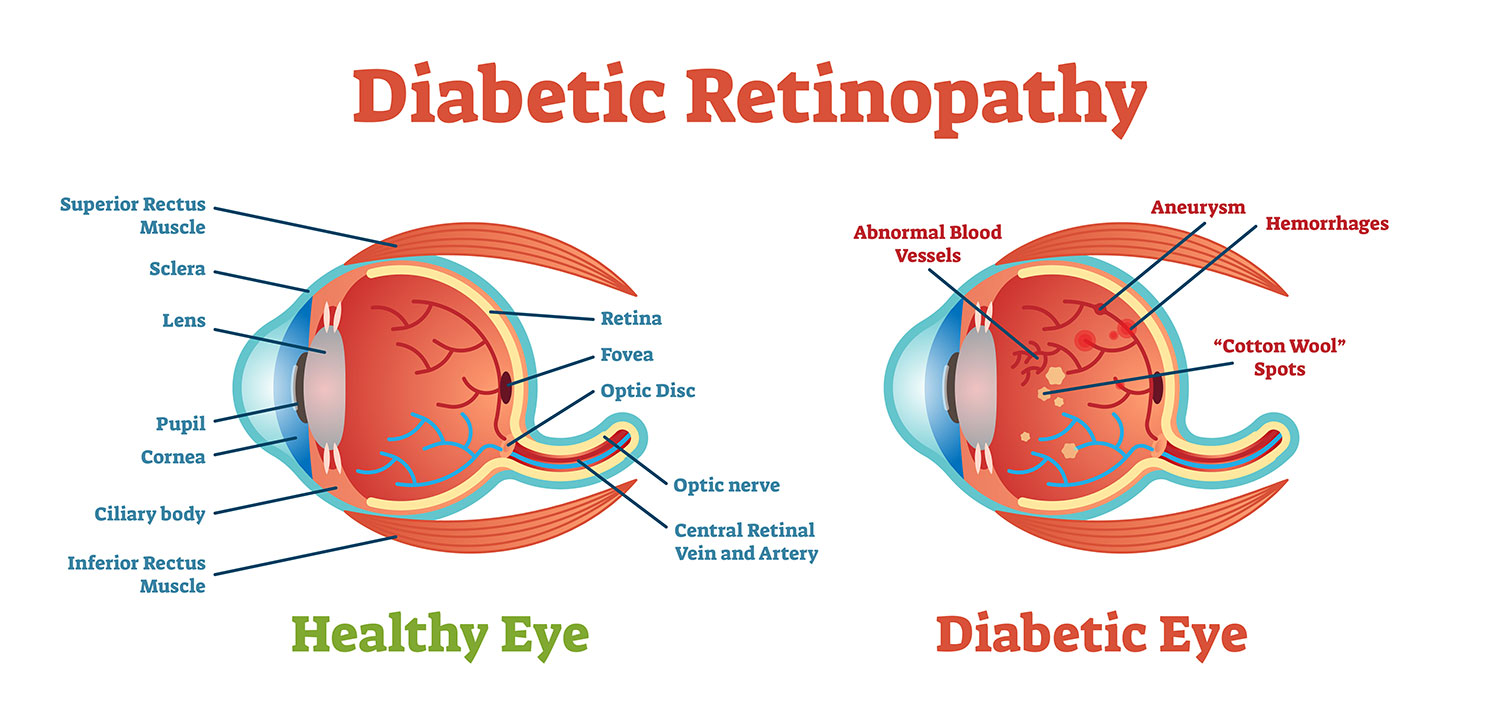
If you have been diagnosed with diabetes, you may be at risk of losing your vision since your body does not utilize sugar properly. When the sugar levels rise, damage to the retinal blood vessels may occur.
This injury to the retinal vessels is known as diabetic retinopathy, and it is the leading cause of blindness in working-age adults. Regular diabetic eye exams are essential to detect these changes early and help protect your vision.
What are the symptoms of diabetic retinopathy?
Often, people may not be aware of any symptoms even when significant diabetic retinopathy is present. As the condition worsens, vision changes can develop and become more noticeable.
Symptoms of diabetic retinopathy may include:
-
Blurry or fluctuating vision
-
Dark or empty areas in your vision
-
The appearance of small specks or larger floaters
-
Colors appearing faded or washed out
-
Sudden vision loss (often from bleeding within the eye)
Macular edema—swelling in the part of the retina responsible for sharp, central vision—can cause persistent blurriness. In advanced stages, abnormal blood vessels may grow and leak, leading to vision loss if not treated promptly.
How is diabetic retinopathy diagnosed?
A comprehensive eye exam by an optometrist or retina specialist is the only reliable means of detecting diabetic retinopathy. After dilating the pupils, a device called an ophthalmoscope is used to view the retina and determine the extent of the retinopathy. If diabetic retinopathy is discovered, a fluorescein dye test and/or optical coherence tomography (OCT) may be recommended.
A fluorescein angiogram involves injecting a dye into an arm vein, then taking intermittent pictures of the retina with a digital camera focused on it for several minutes. OCT is a non-invasive procedure that produces a detailed cross-sectional picture of the macula.
What is the treatment for diabetic retinopathy?
The best therapy for diabetic retinopathy is prevention. Studies show that maintaining strict control of blood sugar levels can significantly lower the risk of vision loss from diabetic retinopathy. It’s also important to treat high blood pressure and kidney problems, as these conditions can worsen retinal damage.
When macular edema or proliferative retinopathy is present, laser surgery is often the first line of treatment. For macular edema, the laser targets leaky areas of the retina to help reabsorb excess fluid. The primary goal of this treatment is to prevent further vision loss. It is uncommon for people to recover significant vision following treatment, but some do experience partial restoration.
Laser surgery is not a cure for diabetic retinopathy and is not guaranteed to prevent further loss of vision. Other treatment options may include steroid injections or a newer class of medications known as anti-VEGF drugs, which help reduce swelling and stop abnormal blood vessel growth.
Get the diabetic eye care you need
If you have diabetes, it’s important to protect your sight with regular eye exams. Schedule an appointment today to have your eyes examined and learn more about your treatment options.